Since the advent of Electronic Medical Records (EMRs), there’s been an overwhelming explosion of data in the healthcare industry. This wealth of information holds immense potential, but it often remains locked away in silos, inaccessible and underutilized. The connection between physicians and patients has now been forever changed, with unintended consequences arising from the disruption caused by “information management solutions.”
In Orthopaedic Surgery, the lack of seamless data integration and visualization has hindered the ability to drive meaningful improvements in patient care and outcomes. However, a new approach is emerging, one that combines the power of in-house data collection, advanced analytics and dynamic visual explainers to help set surgical workflows on the right track.
The rise of same-day surgery in orthopaedics
The demand for same-day surgery has shifted the Orthopaedic Surgery landscape. According to a report by the Ambulatory Surgery Center Association, the number of outpatient surgeries performed in ambulatory surgery centers (ASCs) has increased by 15% annually over the past five years. This trend is expected to continue, with orthopaedic procedures leading the way.
Same-day surgery offers numerous benefits, including reduced costs, improved patient satisfaction, and enhanced efficiency, but it carries unique challenges that only data-led solutions can adhere to seamless data integration, efficient workflow management, and real-time analytics. While these pain points can seem disconnected, there is in fact an easier avenue to consolidate a remedy all in one place.
A unified solution for Orthopaedic Surgery
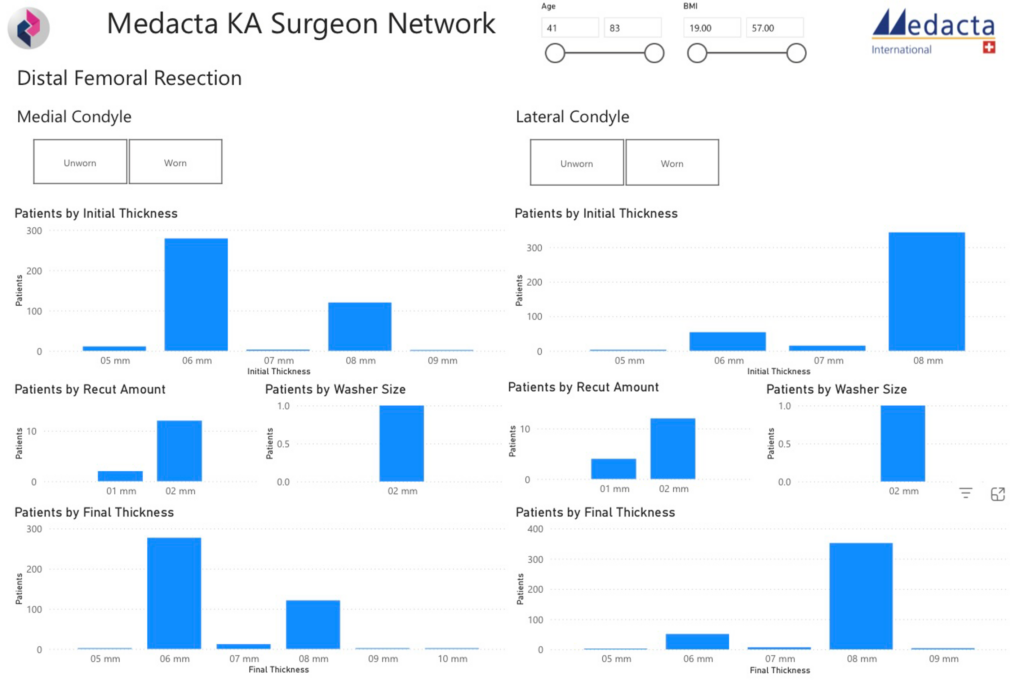
Our innovative platform, powered by PROMs, eOpNote, and barcode scanning, creates a prospective dataset that is dynamic and valuable, in that it facilitates rapid visualization and process improvement. This integrated system captures every real-time insight into the surgical workflow, from implant utilization to variables affecting outcomes, and even opportunities for improvement.
Better data-driven decision making
The key to unlocking the full potential of this data lies in its clearly mapped-out visuals and its subsequent analysis. Our team has developed cutting-edge data display functions that create real value for Orthopaedic Surgeons and patients alike, and by leveraging advanced analytics and machine learning, we can identify patterns, trends, and correlations that were previously hidden.
With our platform, Orthopaedic Surgeons can now:
- Track implant utilization and optimize inventory management
- Identify high-risk patients and develop personalized treatment plans
- See variables that impact patient outcomes and adjust their approach accordingly
- Visualize complex data in real-time, enabling data-driven decision making
- Optimize surgical techniques and reduce complications
- Increase patient throughput, reduce errors, and streamline billing cycles
- Enhance supply chain management and reduce costs
- Improve patient satisfaction and reduce readmissions
The future of Orthopaedic Surgery is patient-centric
A more efficient, effective healthcare system relies on a stronger focus on patients. Luckily, transforming the challenges set by data-heavy EMRs are being solved by capturing data to gain invaluable insights from advanced analytics and innovative visualization methods.
Our platform is at the forefront of this change. Surgeons and healthcare operations staff already face a tough job, but technology can step up to empower them to make data-driven decisions, improve patient outcomes, and drive meaningful improvements in the surgical workflow. It marks a turning point in the way that Orthopaedic Surgery continues to evolve, and we are committed to push the boundaries of what is possible in improving patient care.
To learn more about how we enhanced the EMRs for Mount Carmel New Albany, check out our case study.